《香港兒童醫院通訊》
母乳庫以愛心滋養危重寶寶

母乳能為嬰兒提供最完善的營養,而對極早產及患有危疾的初生嬰兒來說,母乳更具醫療效用,能預防感染和併發症,拯救生命。香港兒童醫院營運全港首個母乳庫,將經消毒處理的捐贈母乳供應至全港公立醫院的新生兒深切治療部,處方給有臨床需要的嬰兒。

《2023年施政報告》宣布建立母乳庫及母乳捐贈機制,醫管局遂成立策導委員會及專家小組等作籌劃。至今年一月,母乳庫投入服務,其總監由本院兒童及青少年科部門主管黃明沁醫生出任。她表示,由於沒有本地經驗可以借鏡,團隊曾到深圳、廣州、新加坡和澳洲的母乳庫取經,參考其設備、運作模式、人手配置甚至宣傳方向等,再按本地情況制訂指引流程。「例如香港的媽媽多數在職,我們便安排速遞公司上門收取母乳,方便捐贈者。」
黃明沁認為,母乳庫負責協調捐贈母乳的收集、處理、篩選、儲存和分配,與本院一向推行的兒科軸輻模式相似,故母乳庫選址在此絕對是相得益彰。
嚴謹程序確保安全衞生
母乳捐贈在香港是一個新概念,不論是捐贈者還是受贈家庭最關心的當然是其衞生及安全。因此,取得公眾的信心極為重要。母乳庫副總監、微生物學家黃卓凝醫生坦言籌備過程中克服了不少挑戰。「我們制訂了符合國際標準的作業流程,更取得ISO 22000及食物安全重點控制系統認證。」

醫務化驗師黃凱蔚補充,部分必需器材在香港連代理商也沒有。她感激醫院採購部積極與生產商溝通,確保母乳庫配備潔淨環境和優質儀器。
捐贈者招募 點滴是愛心
母乳庫能順利啟航和維持恆常服務,關鍵是有充足和持續的母乳來源。母乳庫兩位資深護師林志愛和黃慧芳便擔起捐贈者招募和支援的重任。她們上任後馬不停蹄製作宣傳品,並聯繫各公立醫院婦產科、兒科,和母嬰健康院的醫護人員在前線邀請授乳媽媽們登記。兩人的日常工作還要與有意捐贈者進行健康篩查面談和安排抽血,成功登記後亦會繼續提供母乳餵哺指導,和定期跟進她們的身體情況。


母乳庫原先的目標是一年收集1,000升母乳,結果半年便達標。截至七月中,已有280多位媽媽登記成為捐贈者,約200名嬰兒受惠。黃明沁非常感恩:「這成績遠超預期,我感受到香港媽媽的愛心,和大家上下一心的力量。我們會努力維持母乳庫的高水平服務,並提高家長對捐贈母乳的接受程度。長遠目標是進行相關研究,提升母乳的品質,並藉母乳庫的成功,讓大眾明白母乳的好處,推動更多人加入餵哺母乳行列。」


捐贈母乳解早產孖女燃眉之急
「當我第一眼看見一雙女兒,便忍不住大哭。她們這麼細小,全身駁滿維生儀器,真的很擔心!」唐太的孖女32周時急不及待來到世上,立即被送到伊利沙伯醫院的新生兒深切治療部。醫護人員建議使用捐贈母乳,父母當時感到猶疑。唐生說:「我起初對陌生人的母乳有偏見,但當看到單張說捐贈母乳含有抗體,可降低早產嬰患壞死性小腸結腸炎的風險,便不再考慮,立即同意了,我只想女兒安全健康。」

唐太表示,當時自己的母乳不夠分給兩個寶寶,捐贈母乳大大緩解了她的焦慮。「捐贈者付出這麼多時間心力去泵奶,很感激她們的愛心和無私奉獻。」最終孖女康復出院,唐太亦「追奶成功」,足夠餵養兩個孩子。
捐贈母乳知多啲
- 捐贈者必須正在餵哺一歲以下的嬰兒,並接受健康篩查面談,和抽血檢驗傳染病。
- 合資格捐贈者需遵從指引收集和儲存母乳,之後由指定承辦商上門收集,以冷鏈運送到母乳庫。
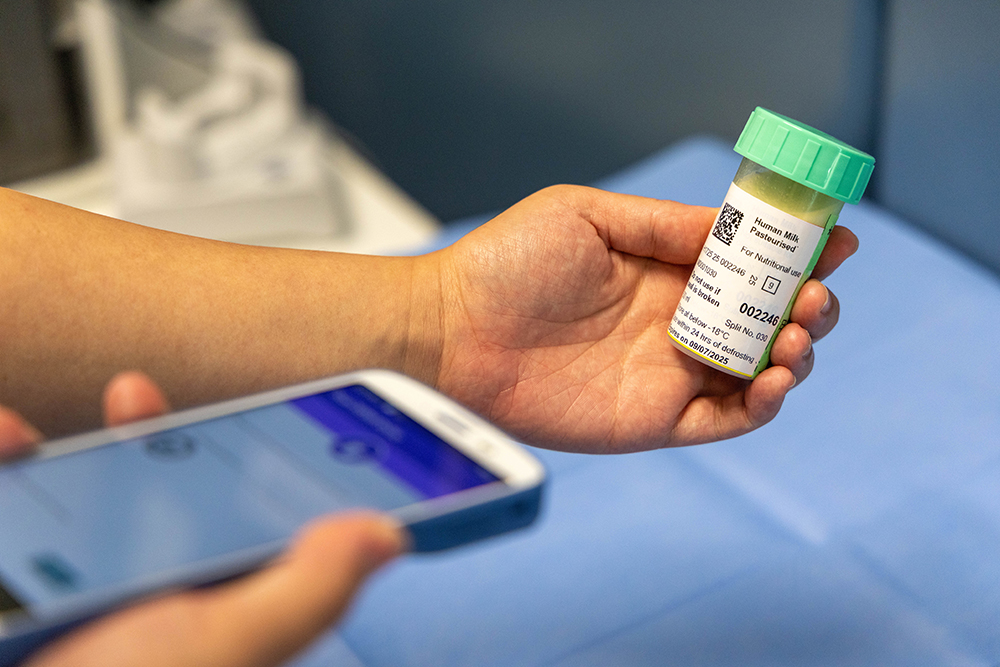
- 母乳運抵母乳庫後經嚴謹處理,包括微生物檢測、巴士德消毒和營養分析,確保安全和品質。
- 經處理的母乳由醫生處方予符合臨床條件的嬰兒,父母需先簽署同意書。






