HKCH Newsletter
Neonatal surgery brings hope to tiny lives

Some babies face life-threatening conditions at birth which require urgent surgery. In 2024/25, the Hong Kong Children's Hospital performed over 80% of the neonatal surgeries of all public hospitals. They are a race against time and testimony to the effort of multidisciplinary teams.
Dr Peter Tam, Chief of Service of the Department of Paediatric Surgery explained, "Neonates who need surgery may be those suffering from congenital anomalies in the digestive system, such as oesophageal, intestinal or anal atresia, which makes feeding impossible. There are also other potentially fatal conditions, including congenital diaphragmatic hernia and necrotising enterocolitis."
Cardiothoracic Surgery Consultant-in-charge Dr Nicholson Yam supplemented, "Some congenital heart diseases such as severe aortic stenosis or total anomalous pulmonary venous connection may cause acute heart failure in newborns and warrant open-heart surgery. We also perform extracorporeal membrane oxygenation support for critical babies."
Specialised skills for challenging operations
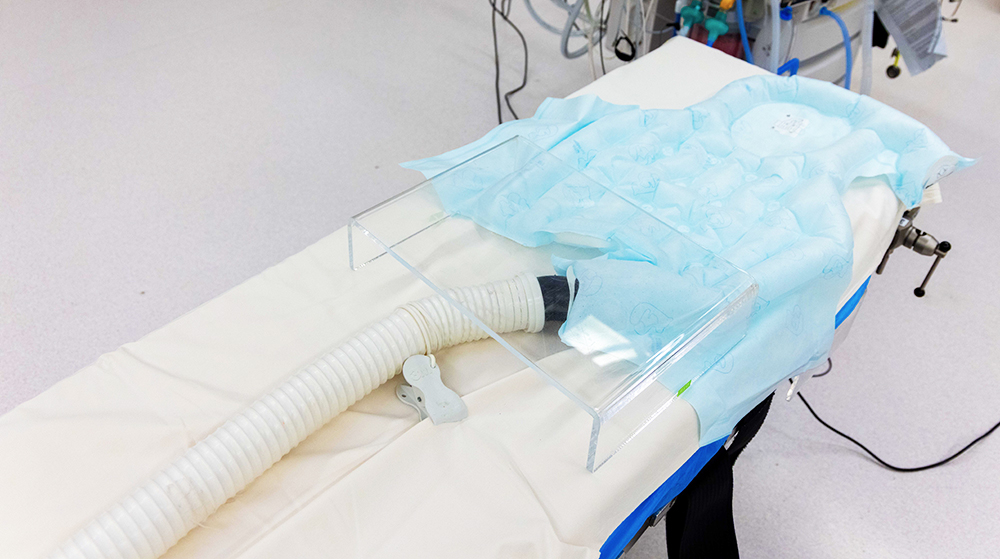
Operating on newborns requires extraordinary surgical skills. Dr Yam said, "Our patients may weigh only a few hundred grams. Their heart could be as tiny as a strawberry and their blood vessels are delicate. Every step demands utmost precision, and we use instruments that are specially designed for neonates." Said Dr Rowena Lee, Consultant, Department of Anaesthesiology & Perioperative Medicine, "Neonates' blood pressure and breathing are volatile. We need to closely monitor their temperature, cerebral blood flow, oxygen level and brainwaves to adjust medications and equipment support. Infants with heart problems usually have variable blood pressure across the body, so multiple arterial catheters are inserted for monitoring."


Dr Tam says, "Neonatal surgeries are rare, complex and ever-changing. Concentrating them in HKCH benefits surgeons' experience accumulation and training, and helps related disciplines to develop teamwork and synergy."
Comprehensive pre- and post-operative care
The neonatal surgery service is not limited inside the operating theatre. A comprehensive system is in place for patient safety and good outcomes. HKCH closely collaborates with the obstetric unit and neonatal intensive care unit (NICU) of regional hospitals. For fetuses identified with anomalies, joint antenatal counselling is provided to formulate treatment plans in advance, and babies can be transferred to HKCH right after birth for surgery.
Consultant of the Department of Paediatrics & Adolescent Medicine, Dr Winnie Chee said, "Our Critical Care Transport Team goes to regional hospitals to pick up babies and escort them during the ambulance ride to monitor their condition and handle any emergencies. Pathway has been cleared so that imaging exams and the operating theatre can be reserved before arrival for a seamless handover. Once we were able to send a 27-week preterm baby with intestinal perforation straight to the NICU operating theatre upon arrival. The operation was performed smoothy, and saved its life."

After surgery, infants are put under close monitoring in the NICU. Healthcare staff will stabilise their heart and lung condition, and pay attention to any signs of hypothermia, dehydration and post-operative complications, to provide appropriate treatment to promote their recovery. Bedside music therapy is also offered in the NICU to soothe their emotions, relieve pain and improve bodily functions.


A high-risk infant programme is also set up where physiotherapists, occupational therapists, speech therapists and dietitians keep track of the babies' development in the post-operative stage and after discharge to provide suitable rehab training.
Baby's first cry touches the heart
"When Kyren was born, he had to be intubated. It terrified me that I didn't hear him cry. Fortunately, he kept improving after surgery. He finally weaned off the ventilator and let out a gentle cry! He is now seven months old and we can treat him like a normal baby. We are beyond grateful to the clinical teams!" Kyren's mother Mrs Yung said blissfully.

Kyren was diagnosed with congenital diaphragmatic hernia when he was still inside his mother's womb. It is a defect involving a hole in the diaphragm which pushes abdominal organs up to the chest, restricting lung development and potentially causing heart failure. The Department of Obstetrics & Gynaecology and peers of the neonatal team of the Prince of Wales Hospital and HKCH teams conducted joint consultation and decided to perform fetal endoscopic tracheal occlusion to save his life. Through the uterus, obstetricians inserted a balloon in the airway of the fetus to help its lungs grow. As soon as Kyren was born, he was transferred to the NICU of HKCH by the Critical Care Transport Team, with the support of inotropes and high-frequency ventilator.
"Once Kyren's condition stabilised after a week, we proceeded with diaphragm repair. The hole was too large that we used his own abdominal muscle flap for closure to reduce the risk of reoccurrence," Dr Peter Tam said.
Kyren gradually recovered and was discharged after over a month, just in time to celebrate Chinese New Year with his family. Looking back at this difficult journey, Mr and Mrs Yung thanked the clinical teams for their exceptional care, "The doctors' clear explanations and confidence in the situation were truly reassuring to us. The nurses also demonstrated professional skills." Dr Tam said, "Despite challenging treatment, parents would never face it alone. We are always by their side."








